If you’ve ever unwrapped a bandage and noticed a smell, you might have asked yourself: “Is this normal healing—or something to worry about?” From both clinical research and real-world wound care experience, it’s clear that odor can sometimes be a natural part of recovery. The key lies in distinguishing between scents that signal healthy progress and those that raise red flags.
In this article, you’ll discover what does a healing wound smell like, what a healing wound can realistically smell like, why odors change during recovery, and how professionals interpret these changes. By the end, you’ll know when to relax, when to pay closer attention, and when to reach out for medical guidance.
Top Takeaways
- Mild, musty, or sweet odors can be normal signs of healing.
- Strong or foul odors often point to infection.
- Pay attention to how the odor changes over time.
- Early medical care prevents complications.
- Odor is a clue, not a diagnosis—professional confirmation is essential.
Healing Wound Odors: Healthy vs. Concerning
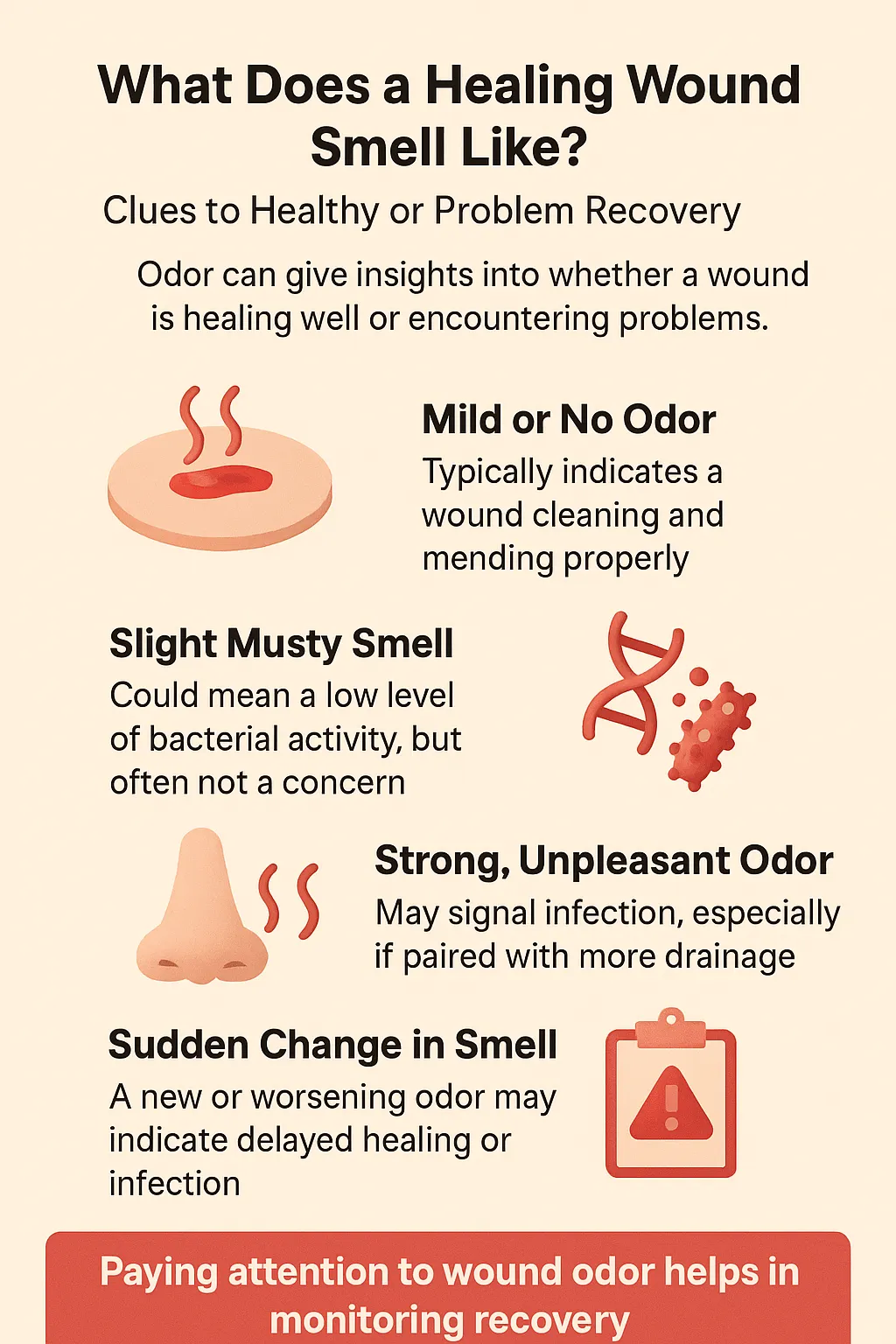
A healing wound may carry a faint scent. Mild, musty, or slightly sweet smells often come from moisture, bandage materials, or the body’s natural tissue breakdown during recovery. These typically fade as the wound closes and skin repairs.
But when odor turns sharp, foul, or increasingly strong, it could indicate infection—especially if combined with swelling, redness, pain, or pus. Healthcare professionals treat odor as a subtle but important clue that helps separate normal recovery from potential complications.
Expert Insight
“In my experience, a mild, musty odor is often harmless. What worries me is when the smell intensifies or changes character and shows up with redness or swelling. That’s one of the earliest signs infection may be taking hold.”
Case Studies & Real-World Examples
Normal Healing After Surgery
- Situation: A post-surgical knee wound gave off a mild, musty smell.
- Observation: No swelling, redness, or pus—just moisture trapped under the bandage.
- Action: More frequent dressing changes and better airflow.
- Outcome: Odor faded as the wound healed.
- Lesson: Not every odor indicates a problem.
When Odor Warned of Infection
- Situation: A patient with a chronic foot ulcer noticed a sharp, unpleasant smell.
- Observation: Odor worsened daily, paired with warmth and pain.
- Action: Early testing, antibiotics, and wound cleaning.
- Outcome: Infection treated successfully, preventing severe complications.
- Lesson: A worsening odor can be the first sign of infection.
Clinical Perspective
- Studies confirm odor, paired with redness or discharge, is a reliable early marker of infection.
- First-hand experience reinforces that it’s the evolution of odor over time that tells the real story.
Supporting Statistics & Insights
- Surgical Site Infections (SSI): Over 110,000 cases reported in U.S. hospitals. A recent CDC update notes infection rates have risen in some categories.
- Pressure Ulcers: Affect 7.5% of nursing home residents, with an estimated $3.3 billion annual cost to the healthcare system.
- Diabetic Foot Ulcers: Lifetime risk is 12–25%, and more than 50% become infected. About 20% of severe cases result in amputation.
- Amputations and Diabetes: Around 60% of lower-limb amputations occur in people with diabetes, with 85% preceded by a foot ulcer.
- Clinical Research on Wound Odor: Odor is strongly linked to bacterial activity. Key diagnostic factors include odor quality, intensity, and progression.
Final Thought & Opinion
- Mild odors usually fade as wounds stabilize.
- When odor becomes foul or is paired with swelling, pain, or redness, it should be treated as a warning.
- My perspective:
- Trust your senses, but don’t rely on smell alone.
- Track patterns and changes over time.
- Seek professional evaluation early if concerned.
Bottom line: Odor is a useful clue, but safe healing comes from combining self-awareness with timely medical care.
Next Steps
- Check for symptoms beyond odor such as redness, swelling, warmth, drainage, or increasing pain.
- Clean and protect the wound by following proper dressing and hygiene practices.
- Monitor changes over time. Note if the odor fades, remains, or grows worse.
- Seek medical help early if the odor worsens or new warning signs develop.
- Rely on professionals for evaluation and peace of mind.
Frequently Asked Questions
Is it normal for a healing wound to smell?
Yes, faint musty or sweet odors can be normal and usually fade as healing continues.
What odor suggests infection?
A foul, strong, or worsening smell, especially with swelling or redness, often signals infection.
Can dressings cause odor?
Yes. Moisture under dressings can create odor even if the wound is healing well.
Is odor alone enough to diagnose infection?
No. Odor must be assessed alongside other symptoms like fever, drainage, or pain.
When should I see a doctor?
Seek care if odor worsens, becomes foul, or appears with new concerning symptoms.
When exploring What Does a Healing Wound Smell Like? Clues to Healthy or Problem Recovery, it’s helpful to think about the importance of a clean, well-maintained environment in the healing process. Just as the body requires balance to heal, your indoor air quality also plays a role in comfort and wellness. Using options like the Payne 19x20x4.25 Air Filters MERV 8 or scheduling professional services such as Air Duct Sealing Service can reduce contaminants that may interfere with recovery. High-quality replacements like the 17.5x23.5x1 Defense Pleated Replacement or bulk options such as the 14x25x1 MERV 8 Pleated HVAC AC Furnace Air Filters (12-Pack) keep the air fresh and supportive of recovery. For affordability and accessibility, platforms like eBay also provide reliable filter solutions that contribute to a healthier environment during wound healing.